Type 1 diabetes and COVID-19
 If you have a child or adolescent with type 1 diabetes (T1D), you probably have questions related to COVID-19. You may have also heard reports suggesting a link between T1D and COVID-19. This document will help answer your questions and concerns.
If you have a child or adolescent with type 1 diabetes (T1D), you probably have questions related to COVID-19. You may have also heard reports suggesting a link between T1D and COVID-19. This document will help answer your questions and concerns.
Can COVID-19 cause type 1 diabetes?
Recent research has found that since the start of the pandemic, the number of children and youth diagnosed with type 1 diabetes has increased in some areas. While this suggests that there could be an association between SARS-CoV-2 (the virus that cause COVID-19) and developing diabetes, it is not yet known if the virus causes diabetes.
We know from pre-pandemic times that there are 2 ways a virus might affect the development of T1D:
- It is believed that a virus may trigger the auto-immune reaction that gradually destroys insulin-producing cells (islets) in the pancreas – the stage known as “pre-diabetes”. Over a period of months to years, the number of islets decreases and at a critical level, blood sugars rise and “diabetes” is diagnosed.
- Some children and youth newly diagnosed with T1D recently had a virus. That doesn’t mean the virus caused diabetes, but the added stress on the body may cause a child with silent “pre-diabetes” to convert to diabetes sooner. These children and youth would have eventually started showing signs of T1D.
It is too early to know whether SARS-CoV-2 is a trigger to develop pre-diabetes or is speeding up an auto-immune process that has already started. It will take months to years of experience and research before we can answer this question.
Researchers have also found that more children and youth are sicker and have diabetic ketoacidosis (DKA) at the time of diagnosis. This is concerning, since DKA is a very serious and potentially life-threatening condition.
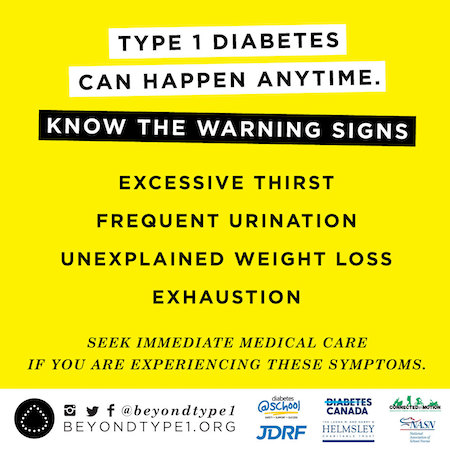
The best way to prevent DKA is to know the signs of untreated or undiagnosed T1D, which are:
- Excessive thirst
- Frequent urination
- Weight loss
- Lethargy
A child or youth with these symptoms should see a doctor right away.
Sometimes the symptoms of undiagnosed T1D are mistaken for flu, a bladder infection, or may show up as bedwetting in a child who was previously dry at night.
Are children with type 1 diabetes at higher risk of serious illness from COVID-19?
Type 1 diabetes is an auto-immune disorder, but this does not mean that people with T1D are immunocompromised or have a weakened immune system.
Fortunately, vaccines prevent serious illness from COVID-19. All children 5 years and older should receive 2 doses of the COVID-19 vaccine, 8 weeks apart. The National Advisory Committee on Immunization (NACI) recommends that youth aged 12 to 17 with underlying medical conditions like type 1 or type 2 diabetes also receive a booster shot (current as of January 28, 2022).
Having any virus or illness can affect blood sugars in people with T1D. Since the chances of high blood sugar and ketones are increased when your child is ill, make sure you are familiar with sick day guidelines. In particular, know:
- How to check for and manage ketones, which can develop with high blood sugar. You can use a blood ketone meter or urine strips. Ensure you have supplies on hand at all times and check expiry dates.
- How to prevent DKA (diabetic ketoacidosis), a serious complication of diabetes caused by not having enough insulin. DKA must be treated in hospital.
- How and when to use mini-doses of glucagon, for children with low blood sugar who are vomiting and cannot take fast-acting sugar. If your clinic hasn’t trained you to do this, ensure you know when to call for help. Have an injectable glucagon kit on hand, even if you have a nasal glucagon product (Baqsimi) as well.
Since anyone with viral symptoms must self-isolate for a period of time, always have a supply of diabetes supplies and medications at home.
How can I prevent my child or youth with type 1 diabetes from developing DKA?
Symptoms of DKA include abdominal pain, nausea, vomiting, high blood sugar and ketones (which cause fruity-smelling breath, and laboured, rapid breathing). Without treatment, DKA can be life-threatening.
Here are some things you can do to prevent DKA:
- If your child is sick and/or has ketones, follow your clinic’s sick day guidelines.
- NEVER stop insulin: During an illness, even if your child is not eating well, insulin needs are usually higher.
- If your child uses an insulin pump, make sure you have either syringes or an insulin pen on hand, in case you need to give fast-acting insulin by injection. Have a supply of basal (long-acting) insulin on hand in case your child’s pump malfunctions.
- Keep your child well hydrated with sugar-free fluids.
- Even if your child needs to isolate in their room, they still need your help to manage their diabetes.
- Even if your child/teen often manages the diabetes fairly independently, during illness or stressful times they will need extra support from you.
- Seek help from your team as directed.
If your child is showing signs of DKA, you need to seek medical attention immediately.
What else can I do?
Do what you can to prevent all family members from contracting COVID-19:
- Get vaccinated: Ensure everyone in your household who can be vaccinated against COVID-19 is up-to-date with those vaccines. Right now, children 5 to 17 should receive 2 doses. NACI (as of Jan. 28, 2022) recommends booster doses for 12-17 year olds with chronic medical conditions including type 1 and type 2 diabetes. Anyone over 18 years should receive 2 doses, plus a booster (3 in total). Contact local public health authorities for information about when and where to be vaccinated.
- Wear properly fitted masks: Remind children to wear their mask securely, both in school and on the bus.
- Stay home when you are sick or having symptoms of viral illness, including COVID-19. Check the website of your province/territory or local public health authority for symptom screening tools.
- Reduce the number of contacts you have, as much as possible.
- Use at-home tests when experiencing symptoms of COVID-19: While supplies of rapid antigen tests (RATs) have recently been limited, provinces and territories are expected to have more available in the coming weeks. In some places, tests will be provided to school staff and students.
- Find out what is happening at your child’s school: Many schools boards have put information about safety measures—including mask availability and ventilation—on their websites.
- Ensure all your child’s vaccines are up to date, including an influenza vaccine.
Additional resources
Last updated: February 2022
